What is a stent?
Stents are artificial devices placed inside tubular structures or organs such as channels, blood vessels, or intestines, usually to relieve or facilitate the healing of conditions like blockages or injuries. Stents can be made of plastic or metal. Plastic stents maintain a constant diameter within the structure they’re placed in, ensuring fluid flow, while metallic ones can expand to a wider diameter within hours of placement.
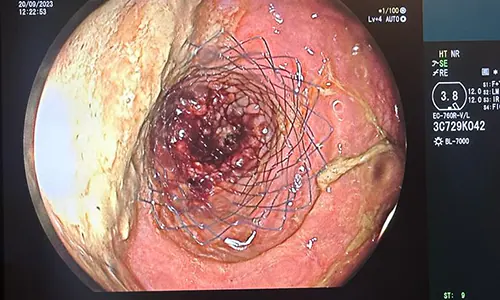
Metal stents are typically compressed into a cylindrical shape and, when the surrounding casing is removed, they expand like an umbrella to sit against the walls of the structure they’re placed in. Depending on their purpose, metallic stents can be used with either a partial or complete impermeable coating or without any coating at all. Intestinal stents are always metallic. Although the term “metallic” implies a rigid structure, they are actually made of bendable, soft, thin wires.
Can a stent be placed in the colon?
Like many parts of the digestive system, stents can be placed in the colon.
Why is a stent placed in the intestine?
Stents can be applied to alleviate a blockage or repair an injured area. In the event of a leak following colon surgery, a portion or the entire area can be covered with a stent to facilitate healing. While there are various methods for healing a leaky area, in suitable cases, applying a stent to the colon can promote recovery.
In colon cancer, stent placement is aimed at relieving the obstruction caused by the tumor in the intestine. Typically, surgery is the primary option for colon cancer even in cases of obstruction. However, in patients with widespread metastasis, where chemotherapy is the primary treatment, a stent can be placed in the colon to initiate treatment as soon as possible. Additionally, in cases where there is no immediate danger of death without urgent surgery, a stent may be placed in the colon as an alternative to performing an open and stomal surgery, allowing for laparoscopic and bag-free surgery instead. Once the intestine is emptied and the edema subsides within about a week, laparoscopic colon surgery can be safely performed.
How is an intestinal stent placed?
In cases of colon obstructions, a gastroenterologist or surgeon typically begins the procedure using a gastroscopy or more commonly a colonoscopy, depending on the distance of the mass from the anus. The endoscopist inserts the device through the anus and advances it to the location of the problem. The endoscope is anchored at a visible gap in the middle or edge of the mass. A special wire is then passed through this gap to advance beyond the narrowing. The pre-compressed stent, depending on the production specifications of the stent and the features of the endoscope used, is then advanced using the special wire previously inserted through the endoscope as a guide. With the assistance of a technician or nurse, the stent sheath is correctly positioned and opened in the right place and manner to ensure that the free stent sits in the lumen.
Alternatively, while the wire is held in place beyond the narrowing, the endoscope device is completely removed, and the stent is directly advanced over this wire. In this method, the colonoscope is again advanced through the anus to place the stent, ensuring it is still performed under direct vision.
After the stent is opened in the relevant area, depending on the obstruction rate of the mass and the resilience of the tissues, attempts can be made to advance the endoscopic device through the stent to the other side of the narrowing. In the presence of a tight stricture or delicate tissue, attempting passage through the stent should be avoided, as it may lead to perforation.
While the basic steps for stent placement for repairing leaks after colon surgery are similar, care must be taken to prevent the leakage area from enlarging. In such cases, coated stents are preferred so that feces can pass through the stent while the exterior coating keeps the leakage area clean. However, coated stents carry the risk of displacement. Therefore, clips called “clips” can be used to secure the stent to the intestinal wall from its edges.
Stent placement can also be considered as a treatment option for strictures developing in old surgical sites or due to inflammatory causes.
Is the patient sedated during colon stent placement?
The procedure is typically performed under sedation administered by an anesthesia team in an endoscopy unit. A patient under sedation is not in a deep enough sleep to not wake up, but they are also in a state where they won’t feel pain or discomfort. The patient naturally wakes up after the procedure.
Depending on the preference of the performing physician or the patient, colon stent placement can also be done under general anesthesia in an operating room setting.
How many days does the patient stay in the hospital after colon stent placement?
If the stent placement procedure is performed safely and there are no other issues requiring the patient to stay in the hospital, the patient can be discharged after waking up from anesthesia and undergoing a physician’s check-up. If there is suspicion of intestinal perforation during the procedure, the patient may be kept in the hospital for observation for a duration recommended by the physician.
Does the colon stent function immediately?
After stent placement for colon cancer, it may take up to 48 hours for the stent to fully expand. Gas and fecal output may begin immediately after the procedure or within hours, depending on the consistency and amount of accumulated feces, the initiation of bowel movements, and the degree of opening of the stent.
Is colon stent placement dangerous?
The most feared complication after applying a stent to the colon is perforation (tearing) of the intestine, primarily due to the tumor. Although the literature reports an increased risk of up to 20%, on average, it can be said that about 7-8 out of 100 patients who undergo stent placement are at risk of perforation. The risk is higher when stents are placed in patients receiving targeted chemotherapy (commonly known as smart drugs) such as bevacizumab.
Additionally, there is a possibility of stent migration. A displaced stent may rarely become lodged in the advanced sections of the intestine, posing a risk of perforation. Although some patients may experience mild and temporary bleeding after the procedure, it is generally not severe.
Similarly, some patients may experience some discomfort after the stent placement, but it is expected to subside quickly. However, if there is severe pain spreading across the abdomen after the procedure, the possibility of perforation should be considered, and the patient should be closely monitored and investigated.
In patients with stents, recurrent blockages may occur due to tumor growth. In such cases, reapplication of the stent may be possible, or surgery may be considered as an option.
What is the cost of colon stent placement?
Stents are mostly imported products and can vary in quality and features. The price of the procedure is determined by the specific product features needed for the patient’s condition.