What is a Rectovaginal Fistula?
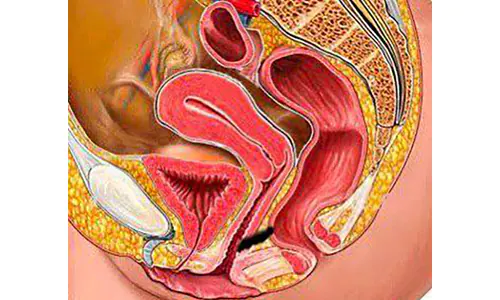
A rectovaginal fistula is the formation of a tunnel or canal between the rectum, the final portion of the large intestine, and the vagina. Through this tunnel, gas and feces may pass from the vagina. It can be considered a significant health problem due to its negative impact on quality of life and the low success rates of treatment.
What Causes It?
The most common cause is trauma during childbirth, accounting for nearly 85% of cases. Additionally, previous surgeries can also lead to rectovaginal fistulas. These may occur after procedures such as rectal surgery, pelvic floor surgery, hemorrhoid surgery, or local tumor excision. Rough sexual intercourse or intercourse with foreign objects can also lead to fistula formation.
It’s also possible for rectovaginal fistulas to develop secondary to rectal or gynecological tumors, as well as due to radiotherapy. Inflammatory conditions such as Crohn’s disease or inflammatory conditions like Bartholin’s abscess can also play a role in fistula formation.
How Is a Rectovaginal Fistula Identified, and What Are Its Symptoms?
The most common symptom is the passage of gas and/or fecal matter from the vagina, either during normal activities or during defecation. In some patients, recurrent urinary tract infections or vaginal infections may indicate an underlying rectovaginal fistula.
How Is It Examined?
In patients presenting with complaints of gas or fecal matter coming from the vagina, a detailed medical history is taken before proceeding to examination. Examination can be performed in the lithotomy position, lying on the left side, or in the knee-chest (prayer) position. During the examination, the fistula tract can be attempted to be felt with a finger through the anus, and the fistula opening can also be felt from the vagina.
In cases suspected of having a fistula, examination and the dye-soaked gauze method can be used as a diagnostic tool. After gently inserting moist gauze into the vagina, the patient is laid on their side. Betadine or methylene blue is applied to the anus, and whether the dye has spread to the gauze in the vagina is checked. To avoid confusion during this examination, the colored fluid should not leak from the anus to the vaginal side. After 1-2 minutes, the gauze in the vagina is removed, and if the color of the substance given from the anus is seen on the gauze, a diagnosis of rectovaginal fistula can be made. However, it should be noted that even if a fistula is present in the patient, there may be no contamination with the colored fluid.
How Is It Diagnosed?
Although diagnosis can be made using the methods mentioned above, the best diagnostic method for rectovaginal fistula is pelvic MRI. Pelvic MRI evaluates findings such as the level, course, presence of accompanying abscess, and whether it affects the sphincters.
Does Rectovaginal Fistula Heal on Its Own?
In some cases, the fistula may heal spontaneously. The rates of spontaneous healing vary depending on the reason for the fistula. Analyses from clinics that see a high number of rectovaginal fistula patients have indicated that non-surgical treatment can be applied to about 20% of patients. Improvement was observed in about 50% of patients who were expected to undergo non-surgical treatment. Therefore, it can be said from these data that spontaneous healing will occur in only about 10% of all rectovaginal fistula cases.
How Is It Treated?
The main treatment for rectovaginal fistula is surgery. The problem can be resolved with appropriate surgery performed by a colorectal surgeon.
What Happens If It’s Not Treated?
If left untreated, a fistula can lead to recurrent urinary tract infections, vaginitis, painful sexual intercourse, or perineal rash. In very rare cases, cancer may develop at the site of the fistula many years later.
Rectovaginal Fistula Surgery
Several techniques have been identified for the treatment of rectovaginal fistula. One of these is the application of a special staple resembling an OTSC (Over-The-Scope Clip) colonoscopically to close the fistula. This staple is expelled through the anus within weeks. Success rates of up to 40% have been reported.
Fistula plugs, which have also been tried for anal fistulas, can be used for rectovaginal fistulas as well. This involves inserting a specially manufactured plug into the fistula to fill it, extending from the vagina to the bowel. Success rates of around 20-30% have been reported.
Although attempts have been made to heal rectovaginal fistulas using special tissue adhesives called fibrin glue, success has only been achieved in about 30% of cases. Stem cell therapy has been tried, particularly for rectovaginal fistulas associated with Crohn’s disease, and improvement has been observed in about 27% of cases.
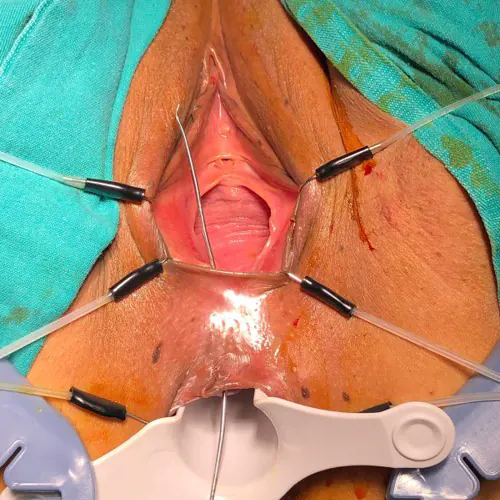
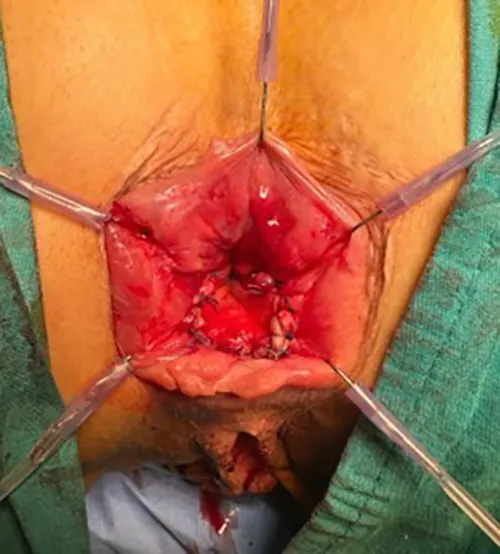
In addition to these local treatments, many surgical methods have been described. Depending on the approach area during surgery, these methods can be categorized into four different approaches: transperineal (entered between the vagina and anus), transvaginal (from the vagina side), transanal (from the anus side), and abdominal (entered through the abdomen). While the goal in all approaches is to eliminate the fistula, the techniques vary.
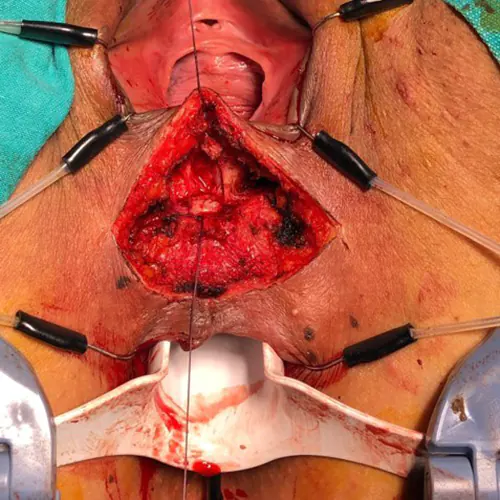
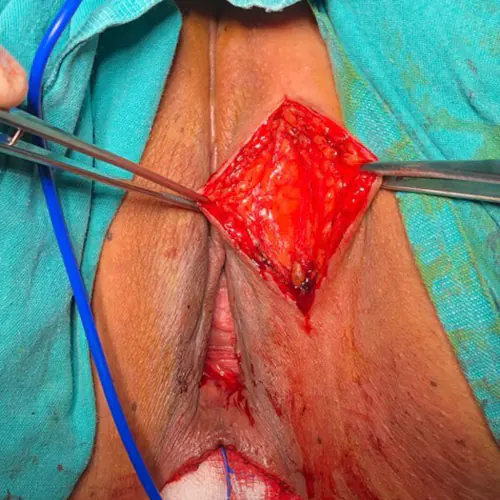
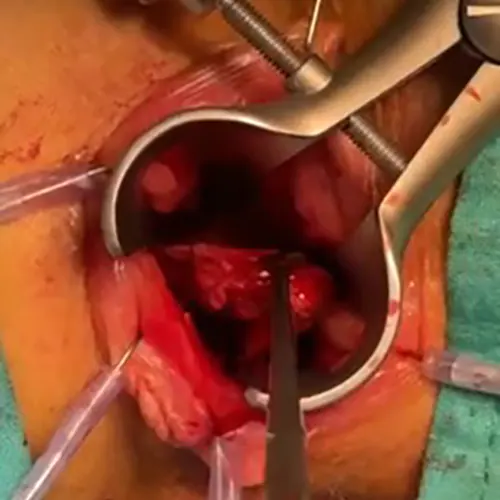
The Martius flap technique has been described as a method used to repair fistulas between the urinary tract and vagina, where a flap of bulbocavernous muscle is used as a filler. Subsequently, a modified Martius flap technique has been described for rectovaginal fistulas. In the modified Martius flap technique, a cut is made in the perineal skin between the vagina and anus, and tissues between the rectum and vagina are separated. After identifying the fistula tract, it is sutured from both sides and cut in the middle to divide the fistula. Subsequently, usually a straight incision is made from the left labium majus (outer lips) to free the subcutaneous fat tissue without disrupting the vascular structure. This fat flap is then spread between the rectum and vagina to separate the fistula. Finally, the incisions made in this area are closed with absorbable sutures. Cuts are present both in the perineum and on the outer lips. Success rates of between 65-100% have been reported.
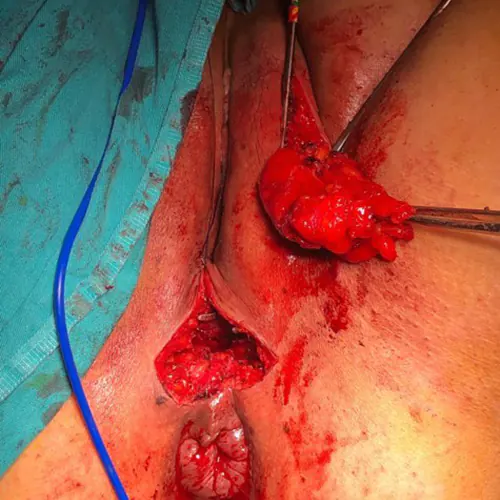
In the method where the gracilis muscle is used as a flap, similar to the Martius flap, after preparing the tissues, the gracilis muscle is used as the flap. The gracilis muscle is a thin, long muscle that extends to the knee. The lower parts of this muscle are freed and cut with incisions made in the thigh. Then, it is passed under the skin and spread into the space between the rectum and vagina, and secured. The incision sites are sutured to conclude the surgery.
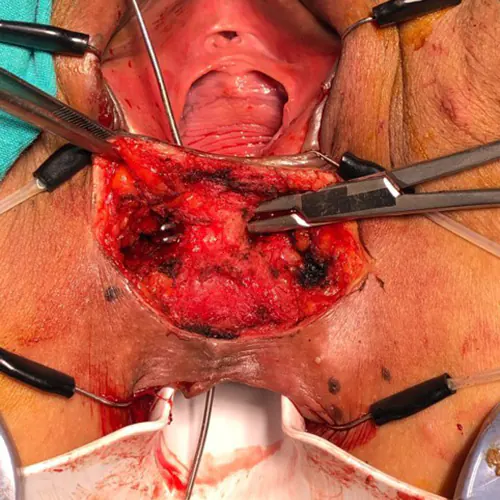
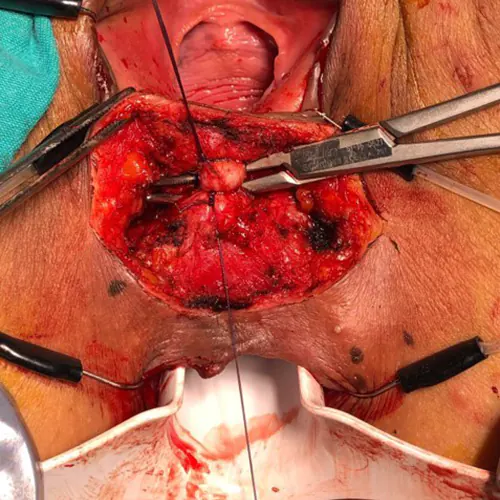
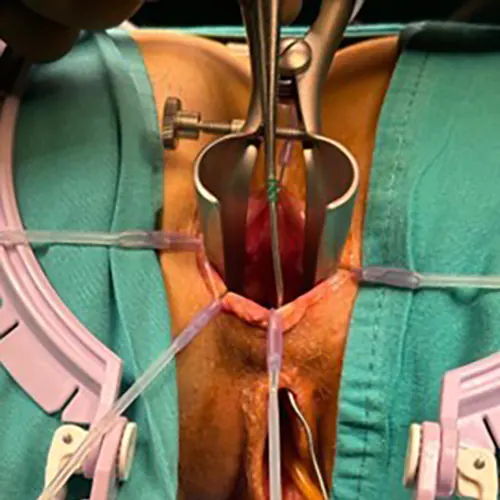
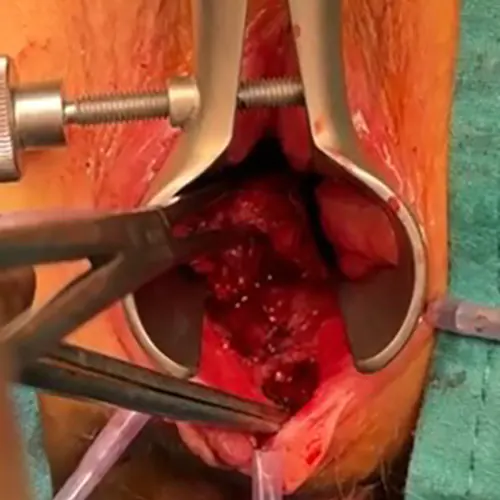
The endorectal advancement flap is a method applied through the anal route. The patient is preferably placed in the prone jack-knife position (lying face down with knees bent). After identifying the fistula tract, similar to the application in anal fistulas, the fistula tract extending from the rectum to the vagina is completely removed as much as possible without damaging the muscle tissue. The rectum wall is lifted upwards for about 4-5 cm. There should be mucosa and submucosa in the lifted wall. Depending on the surgeon’s preference, there may be some amount of muscle tissue. It is even possible to lift the entire rectum wall. The lifted flap can be in the form of a broad-based V or U shape. The prepared flap should be tension-free to be sutured smoothly under the dentate line. At this stage, the area from which the fistula is removed is tightly closed with absorbable stitches. Then, the prepared flap is sewn onto the anal mucosa with absorbable stitches in a regular manner. There is no visible incision on the patient in this method. The healing rate of the fistula is reported within a wide range of 42-78%. Success rates are influenced by factors such as the tension of the flap, ischemia of the tissue, the cause of the fistula, and whether the patient has additional diseases.
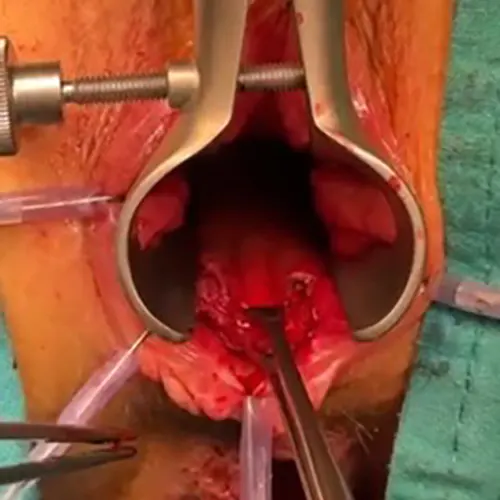
In classical fistula surgery, as done in traditional methods, the cutting of all muscles until reaching the fistula can also be considered. After cutting the muscles and exposing the fistula, the fistula tissue is removed. The sphincter muscles can be repaired by suturing them back together with absorbable or non-absorbable stitches, depending on the surgeon’s preference. After repairing the mucosa on both the rectum and vagina sides, the skin is sutured to conclude the surgery. Healing rates have been reported as 78-100%. However, it should be noted that in patients with birth injuries undergoing sphincter repairs, there is a possibility of developing sphincter dysfunction over time, as the effectiveness of the repair may diminish.
For high-positioned fistulas, an abdominal approach is generally preferred. Open, laparoscopic, or robotic techniques can be applied. The basic principle is the removal of the tissue causing the fistula and closure of the vaginal side. The removal of the tissue causing the fistula usually involves a procedure requiring anastomosis in the small intestine, colon, or rectum. Therefore, there is a possibility of leakage and recurrence of the fistula. In an attempt to prevent this, abdominal fat tissue called omentum is spread between the vagina and tissues. Success rates have been reported around 50%.
The surgeon will choose the most familiar and successful method personally, considering factors such as the characteristics of the tissues, whether the fistula is close to the anus or positioned higher, the presence of active infection, and the cause of the fistula development.
Is a Stoma Created in the Treatment?
The opening of a stoma is a approach that can be considered at every stage in the treatment of rectovaginal fistula. It has been observed that spontaneous healing can occur if there is a stoma opened in the first surgery for fistulas developing after rectal surgery. In cases where a stoma was not opened in the first stage after rectal surgery and a rectovaginal fistula develops, opening a stoma as an ileostomy or preferably colostomy can promote spontaneous healing.
Additionally, a surgeon applying the aforementioned methods may decide to open a stoma in addition. The aim here is to keep the surgical area dry and clean, thus increasing the healing rates. When making this decision, the benefits of opening a stoma should be compared with the psychological impact it may have on the patient, and a decision should be made on a case-by-case basis.
How Long Does Rectovaginal Fistula Surgery Take?
The duration of the surgery can vary between 20 minutes to 180 minutes, depending on factors such as the technique applied, the surgeon’s experience and dexterity in this field, the presence of obesity in the patient, and the presence of fibrosis due to previous surgeries.