What is a tailgut cyst?
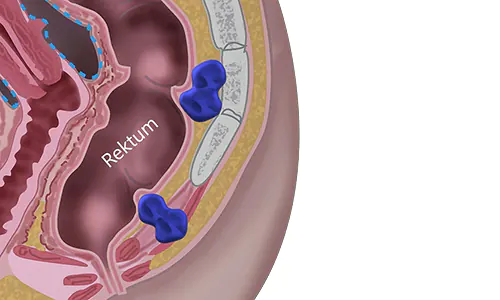
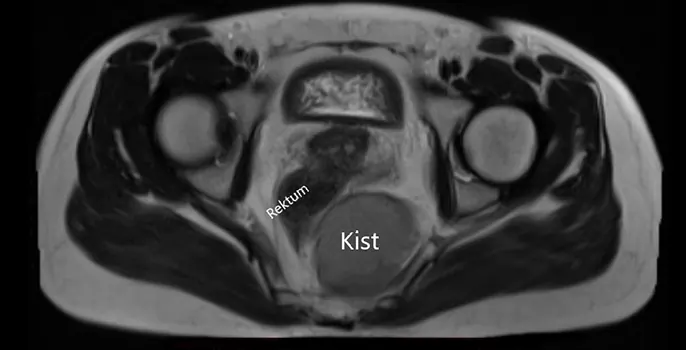
Tailgut cysts are rare congenital (present at birth) lesions. It is estimated that one in 40,000 births will have a tailgut cyst. They are typically found behind the anus-rectum junction. Based on their location, they can be grouped with other lesions as retrorectal (located behind the rectum) or presacral (located in front of the sacrum) lesions. Tailgut cysts are also referred to as retrorectal cystic hamartomas.
Although they are known to be congenital lesions, patients often receive a diagnosis in adulthood. They are observed three times more frequently in females than in males. The reason for diagnosis in later ages is twofold: some tailgut cysts remain asymptomatic, while in some patients, symptoms are not attributed to a tailgut cyst, leading to a lack of further investigation.
What are the symptoms of a tailgut cyst?
In nearly half of the patients with a tailgut cyst, there are no symptoms. They are often detected incidentally during radiological examinations conducted for other reasons. In other patients, symptoms may arise due to the pressure of the cyst on surrounding organs or due to infection. While originating from behind the rectum, as the cyst enlarges, it can exert pressure not only on the rectum but also on organs such as the vagina and bladder. A tailgut cyst can cause symptoms such as frequent urination and burning sensation during urination due to pressure on the bladder, as well as a sensation of fullness in the rectum, painful or difficult bowel movements, narrowing of the stool, and constipation due to pressure on the rectum. Because of its space-occupying nature in the retrorectal area, individuals may feel discomfort in the buttocks and coccyx region while sitting, and they may have difficulty sitting comfortably. When infection occurs in these cysts, it can manifest as a pelvic/anal abscess, painful swelling in the anal area, and in some cases, as a fistula.
How is a tailgut cyst diagnosed?
In patients presenting with specific complaints, suspicion of a tailgut cyst may arise during a rectal examination when a mass effect is felt externally behind the rectum, or during a gynecological examination when a cystic lesion is seen on ultrasound. However, the radiological diagnosis of a tailgut cyst is usually made with pelvic MRI. Although a cystic structure may be seen on computed tomography in some patients, MRI is often the preferred radiological diagnostic method for the complete characterization of the lesion. Biopsy of lesions suspected to be tailgut cysts is not recommended.
Does a tailgut cyst turn into cancer?
In the medical literature, malignant transformation on the basis of a tailgut cyst has been reported in many cases, but it is not known exactly how many of these cysts carry the risk of developing cancer. Delay in diagnosis or failure to perform adequate surgery is thought to increase the risk of cancer development.
What is the treatment for a tailgut cyst?
There is no medication for treatment. Surgical removal of the cyst is necessary. Surgically removing the cyst allows for a definitive diagnosis of the suspected disease, resolution of any symptoms the patient may have, and elimination of the risk of cancer development. Extensive surgical intervention is required for tailgut cysts that have developed cancer, similar to any cancer, while for cysts that have not developed cancer, simply removing the cyst is sufficient.
How is surgery for a tailgut cyst performed?
The surgical approach is determined based on the level of the cyst. For cysts located well above the pelvic muscles, an abdominal approach, either open or laparoscopic, may be preferred. If the cyst is located below the pelvic muscles or in an easily accessible area, a posterior (back) approach may be used. In some patients, surgery may need to be performed from both sides.
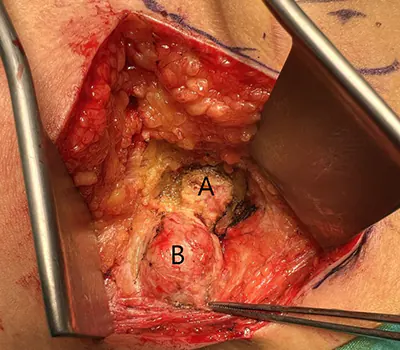
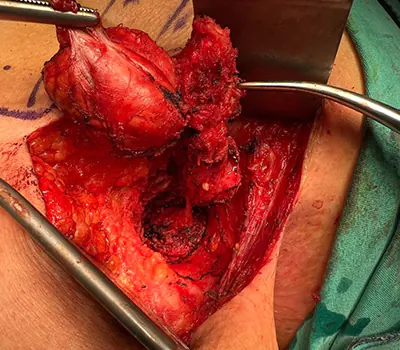
During the abdominal approach, the surgeon carefully separates the cyst from the rectum, sacrum bone, and, in some cases, the vagina or pelvic muscles, and removes it outside the abdomen in a sterile bag. Maximum care should be taken during this separation process to avoid damage to the rectum, vagina, and surrounding blood vessels. In case of any injury, effective repair should be performed.
In the posterior approach (Kraske approach), with the patient in a prone position, an incision is made through the skin and fatty tissues from the side of the sacrum bone and coccyx (tailbone). After cutting the anococcygeal ligament, the cyst is accessed. In some patients, the coccyx bone may need to be removed at this stage due to reasons such as the need to expand the working area or adhesions of the cyst. Once the cyst is exposed, it is completely removed without causing damage to the levator muscles or rectum and leaving no tissue behind. Depending on the size of the field, the nature of the tissues, and the surgeon’s preference, a drain may be placed in the surgical area. Subsequently, the layers are sutured layer by layer to conclude the operation.
In a combined approach, part of the surgery can be performed abdominally while the rest is done from the back, or vice versa, using the same principles and techniques.
Is surgery for a tailgut cyst risky?
Surgery for a non-malignant tailgut cyst, when performed by experienced hands, is not considered to carry significant risks. However, in cases where malignancy has developed, in patients who have previously had infections, or when surgery is performed by individuals lacking sufficient experience, complications such as rectal injury, vaginal injury, urinary tract injury, vascular injury, residual disease, or damage to the anal sphincter or pelvic muscles may occur. If these problems are not effectively addressed, long-term complications such as recurrence, fistula, or fecal incontinence may develop.
What is the cost of surgery for a tailgut cyst?
The cost of surgery is calculated based on factors such as the duration of the surgery, whether the patient has had previous interventions in the same area, whether the surgery is performed abdominally or posteriorly, and whether malignancy is present.
Recovery after surgery for a tailgut cyst
If the surgery is performed safely without any damage to the rectum or other surrounding organs, one night of hospitalization is usually sufficient. If repair of possible damage to surrounding organs is performed, the patient may need to be hospitalized for observation during the recovery period, which can extend up to 4-5 days. After complete recovery, patients can resume their normal activities without any issues.
Follow-up after surgery for a tailgut cyst
If there are no findings suggestive of malignancy in the cyst removed during surgery and sent for pathological examination, patients do not require any additional treatment. Since recurrence is not expected if the cyst is completely removed, no radiological or clinical examination/control is necessary. However, if the cyst is not completely removed, the surgeon may recommend periodic follow-ups based on the patient’s characteristics. There is no universally accepted follow-up algorithm for this purpose.