In today’s world, we frequently encounter gallbladder problems due to both dietary habits and systemic diseases. It is important to be informed about how gallbladder and bile duct diseases develop, the symptoms they present, and the treatment methods for prevention and timely medical intervention if necessary. On this page, you can find information about gallbladder and bile duct anatomy, diseases, risk factors, symptoms, and treatment methods.
What is the gallbladder and bile duct?
The gallbladder is a hollow organ located under the liver, adhered to one side of the liver by connective tissue, shaped like a pear, and connected to the main bile duct with a channel. Bile is produced in the liver and is delivered to the gallbladder through bile ducts. Therefore, the gallbladder is an organ that stores, rather than produces, bile. Particularly after the consumption of fatty meals, the gallbladder contracts due to the effect of certain hormones, releasing the bile into the bile duct. The bile reaches the intestine from there and mixes with the ingested food. This meeting is crucial for digestion.
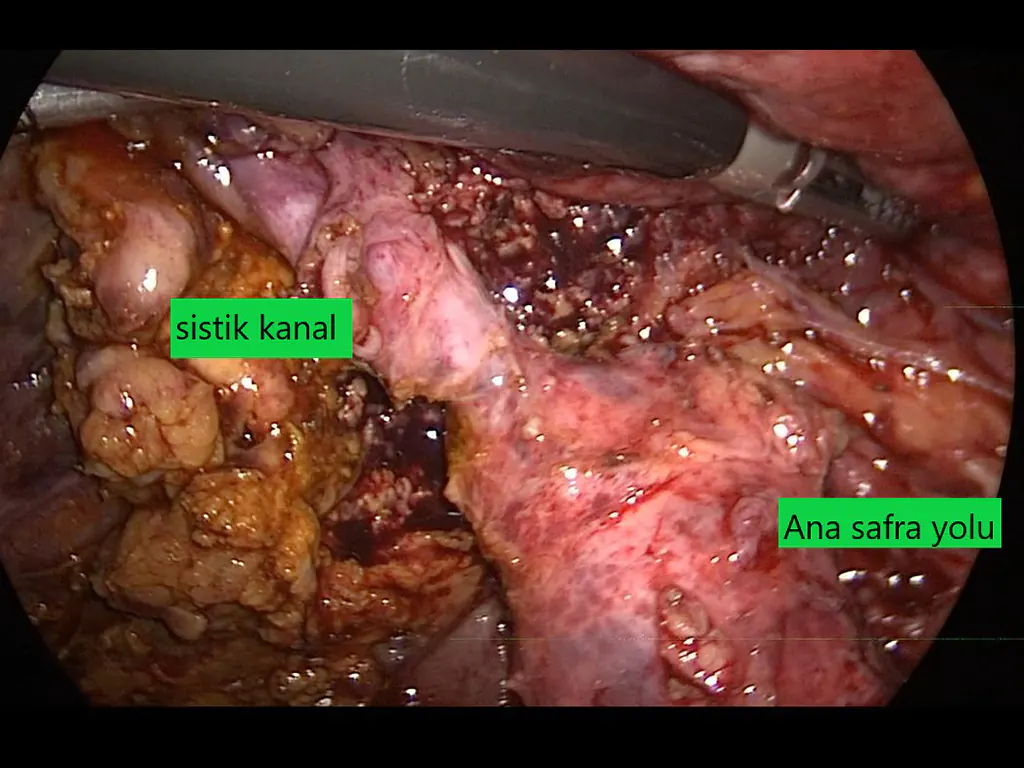
We can liken the bile ducts to a large tree. Very small bile ductules embedded within the liver merge at several levels to form larger channels. In the final stage, the right main bile duct and left main bile duct exit the liver on the right and left sides, respectively, joining each other outside the liver. This joining creates the main bile duct, which we can describe as the trunk of the tree. A few centimeters below this, the gallbladder duct (cystic duct) connects to the bile duct. Below this level, the bile duct is referred to as the common bile duct. After continuing for a bit, the common bile duct passes behind the duodenum (the first part of the small intestine) and immediately enters the pancreas at this level. Often, it merges with the main pancreatic duct, reaching the duodenum 1-2 cm later.
What are gallbladder and biliary tract diseases?
Diseases that may develop in the gallbladder:
- Gallstones/sludge
- Acute cholecystitis (inflammation of the gallbladder)
- Gallbladder polyps
- Gallbladder cancer
Diseases that may develop in the bile duct:
- Bile duct obstruction (obstructive jaundice)
- Acute cholangitis (inflammation of the bile duct)
- Bile duct injuries
- Bile duct strictures
- Bile duct tumors
Why do gallstones form?
Environmental and genetic factors can play a role in the formation of gallstones. In individuals with a family history of gallstones, the likelihood of developing stones is found to be around 15%, compared to about 3% in those without stones. Therefore, hereditary transmission is considered. Genetic predisposition is not overlooked, and it should be noted that similar lifestyles and dietary habits in these individuals can also contribute to the formation of gallstones.
Gallstone formation is more commonly observed in women and increases with age.
Pregnancy has been identified as a risk factor for gallstone formation. In fact, the frequency of gallstones increases with the number of pregnancies.
Although the exact cause is not fully understood in individuals with diabetes, gallstone formation is more common.
Gallstones are more prevalent in obese individuals, and conditions such as gallstone-related pain and infections are also more frequent. Additionally, rapid weight loss has been observed to increase the formation of gallstones and related symptoms. Many individuals undergoing obesity surgery such as sleeve gastrectomy or gastric mini-bypass end up having gallbladder surgery over the years due to rapid weight loss.
Some medications are known risk factors for gallstone formation. Cholesterol-lowering drugs containing fibrates, antibiotics containing ceftriaxone, medications containing octreotide, and the use of estrogen hormones can lead to the formation of gallstones.
Cholesterol stone formation is triggered in patients receiving total parenteral nutrition, which refers to nutrition delivered through intravenous feeding.
Gallstones are more common in individuals with Crohn’s disease or those who have had the last part of the small intestine removed surgically.
In patients with liver cirrhosis, gallstones are more frequently detected compared to those without cirrhosis.
Individuals with blood disorders such as sickle cell anemia, thalassemia, and hereditary spherocytosis are at an increased risk of gallstone formation.
What are the symptoms of gallstones?
Many individuals with gallstones may not be aware of their condition as they do not experience any problems. The majority of those who are incidentally diagnosed with gallstones during radiological imaging for other reasons do not describe any specific symptoms. The most common complaint related to gallstones is a condition called biliary colic. In this situation, the patient experiences intense, discomforting pain in the upper right side of the abdomen, just below the right ribs, and sometimes in the upper middle part of the abdomen. This pain can also be felt in the back on the right side and even in the right shoulder. In addition to pain, nausea, vomiting, and profuse sweating may occur. Although this pain typically occurs after a fatty meal, some individuals may experience the same pain independent of meals, even during the night. The pain, lasting for at least 30 minutes, does not diminish with changes in position such as sitting or standing or activities like passing gas and can last up to 6 hours.
Sometimes, symptoms related to complications of gallstones may also occur. These complications may include acute cholecystitis (inflammation of the gallbladder), gallstone in the bile duct, cholangitis (inflammation of the bile duct), pancreatitis (inflammation of the pancreas), Mirizzi syndrome, gallstone ileus, or gallbladder cancer.
Should gallstones be surgically removed?
Patients with symptoms and/or complications of gallstones are recommended to undergo surgery. In cases where there are gallstones detected incidentally without any symptoms, a selective approach should be taken. Gallstones without symptoms have been found to develop symptoms within a period of 10-15 years with a probability of only 15-25%. On the other hand, the probability of developing complications such as cholecystitis, cholangitis, and pancreatitis is found to be around 2-3%. Therefore, if gallstones that do not cause any problems are not surgically treated, the individual will likely continue to live without issues with a 75% probability. Since it is not possible to predict which patients with no problems will start experiencing issues due to gallstones, the decision for surgery can, to some extent, be left to the patient. While one individual with gallstones may choose surgery as a precaution against the possibility of developing problems, another individual may prefer to wait, considering the risk to be low.
Is the gallbladder completely removed?
In gallstone surgery, the gallbladder is completely removed. There is no practice of only removing the stones and leaving the gallbladder in place. Although a team in China experimented with such a method, it was not deemed appropriate due to negative results. Therefore, in gallstone or gallbladder inflammation surgeries performed worldwide, the entire gallbladder is removed.
What happens if the gallbladder is not completely removed in gallbladder surgery?
The gold standard treatment for patients experiencing issues related to gallstones is cholecystectomy, the surgical removal of the gallbladder. The ideal approach in this surgery is the complete removal of the gallbladder.
But what if, despite the intention to remove it entirely, a part of the gallbladder remains?
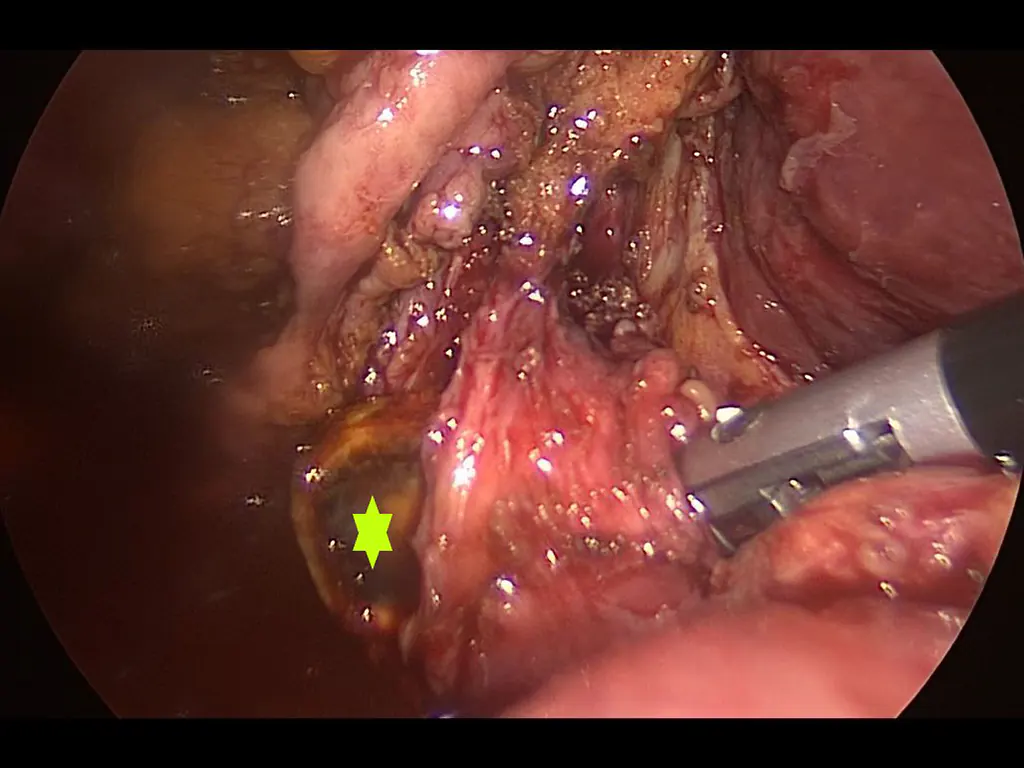
Interestingly, the situation where the gallbladder cannot be completely removed, which was rarely seen in the era of open cholecystectomy, is now reported more frequently after laparoscopic cholecystectomy.
This poses a noteworthy issue considering the many advantages of laparoscopic surgery. Leaving the base of the gallbladder or an excessively long cystic duct after laparoscopic cholecystectomy can result in the persistence or recurrence of patients’ complaints.
In a patient who has undergone cholecystectomy but had the gallbladder left as if no surgery had been performed, symptoms such as abdominal pain, indigestion, nausea, and even jaundice may occur. Additionally, complications like cholangitis (inflammation of the bile duct) or pancreatitis (inflammation of the pancreas) can develop. The cause of these complaints may be the presence of remaining stones in the residual gallbladder portion or the formation of new stones over time.
The incomplete removal of the gallbladder during laparoscopic cholecystectomy has been reported in some series to be around 13%. In other words, the gallbladder may not be completely removed in about one out of every 7-8 patients undergoing gallbladder surgery. Several risk factors have been identified for the development of this situation:
- The gallbladder bed not being accurately placed during surgery,
- Previous surgery or intense adhesions due to inflammation,
- Active gallbladder inflammation (acute cholecystitis),
- Excessive bleeding during surgery impairing visibility,
- Congenital gallbladder anomaly,
- Changes in anatomy due to lesions developing later in the gallbladder.
In cases where patients continue to experience symptoms despite gallbladder surgery, the sole problem is not the remaining gallbladder portion. However, specific tests should be conducted to either exclude or confirm this possibility. While initial tests may include blood tests and ultrasound, in many patients, magnetic resonance cholangiography (MRCP), a type of MR imaging of the bile duct, is crucial for diagnosis. In some cases, diagnosis occurs during endoscopic retrograde cholangiopancreatography (ERCP), an endoscopic procedure to examine the bile duct.
If appropriate tests show no stump or stones left, other potential causes for the symptoms should be investigated. On the other hand, if a residual gallbladder or a stone within a long cystic duct is detected, intervention is usually necessary. These interventions can be endoscopic procedures or a repeat surgery, either open or laparoscopic. As anticipated, subjecting a patient to repeat surgery poses a risk of bile duct injury, vascular injury, or damage to other organs.
Although the likelihood of not completely removing the gallbladder is considered lower with increasing experience, it continues to be a significant problem in terms of clinical importance. As in any surgery, having a deep anatomical knowledge and high expertise in challenging cases is crucial for the complete removal of the gallbladder and to avoid such issues.
Is gallbladder surgery risky?

Laparoscopic gallbladder surgeries are commonly performed in today’s general surgical practice. It is often perceived by many patients as a simple procedure, although not as challenging as cancer surgery, gallbladder surgeries are considered specialized operations. This is because certain complications (problems) that may arise during or after the surgery can negatively impact the patient’s life.
Complications such as injury to the bile duct, vascular damage, and intestinal injury can occur during gallbladder surgery.
Bile duct injury is the most feared complication, as it can lead to bile leakage, bile stasis, and progression to cirrhosis. Additionally, it can result in the need for endoscopic interventions or repeat surgery after the procedure.
Vascular injury can occur to the hepatic artery or portal vein, which carries blood to the liver. Especially in cases where bile duct and vascular injuries occur, the risk of death or the need for liver transplantation is higher.
In some patients, injury to the duodenum (the first part of the small intestine) and the large intestine can occur. Complications are more common in patients who have undergone abdominal surgery, had gallbladder inflammation, and/or are obese.
Scientific data indicates the importance of an experienced surgeon and appropriate surgical technique in minimizing such complications.
How long does gallbladder surgery take?
The duration of laparoscopic gallbladder surgery can be influenced by factors such as the patient’s intra-abdominal fat, gallbladder inflammation, intra-abdominal and gallbladder adhesions, liver size, surgical experience, and operating room equipment. In an ideal patient with all conditions favorable, where the surgeon starts by making an incision in the skin, removes the gallbladder, and closes the skin again, the procedure can be as short as 15 minutes, but it can extend to up to 3 hours in some cases. When adding the time for administering anesthesia and waking up the patient, a gallbladder surgery generally takes around 45-60 minutes.
What is the cost of gallbladder surgery?
Factors determining the difficulty of the surgery also affect the surgery cost. An increase in surgery time and the need for specialized materials can lead to an increase in the surgery cost. Relevant departments calculate the surgery cost taking into account the patient’s characteristics.
What is gallbladder inflammation?
Gallbladder inflammation (acute cholecystitis) is an infection that typically occurs in individuals with gallstones. Symptoms include nausea, vomiting, fever, and abdominal pain below the rib cage. The abdominal pain can be felt in the back, between the shoulder blades, and in the right shoulder. These symptoms are usually severe enough to prompt the patient to the emergency room or surgical clinic. However, some patients may experience gallbladder inflammation without seeking medical attention due to a high pain threshold, using painkillers at home, or having mild symptoms.
Is gallbladder inflammation dangerous?
If gallbladder inflammation is timely and properly treated, it can be considered a relatively harmless condition. However, if left untreated, it can lead to a serious infection state known as sepsis. Sepsis can be fatal if not treated correctly and adequately.
In patients with gallbladder inflammation, gallbladder perforation and the spread of bile into the abdominal cavity can occur. This condition can lead to sepsis and be fatal.
In some cases, accompanying conditions like cholangitis and pancreatitis with gallbladder inflammation can negatively impact the patient’s overall health, leading to life-threatening health problems.
Treatment of Gallbladder Inflammation
As gallbladder inflammation is a bacterial infection, it is treated with antibiotics. In addition to antibiotics, pain relievers, anti-nausea drugs, and antispasmodic medications are also used. With these medications, gallbladder inflammation can be treated within a few days, but sometimes bringing the disease under control can take weeks.
Alternatively, urgent laparoscopic surgery can solve the problem by removing the gallbladder. Although gallbladder inflammation can be treated, recurrent infection attacks in patients, frequent colicky pains, and the increased difficulty of surgery after repeated attacks have led to urgent cholecystectomy being considered the primary treatment for gallbladder inflammation nowadays. However, in patients with systemic diseases or gallstone complications severe enough to prevent surgery, medication is prescribed instead of surgery. In these patients, gallbladder surgery is recommended again after the underlying problems have been resolved.
While gallbladder inflammation surgery provides a quick and definitive solution, there are some concerns about the timing. Many surgeons prefer to avoid surgery if three days have passed since the onset of abdominal pain. They believe waiting 6-12 weeks under medication treatment is necessary instead of opting for surgery. However, current scientific data and personal experience indicate that if there is no other condition preventing surgery, gallbladder surgery can be safely performed at any time after the onset of pain.
Is Gallbladder Surgery Risky After ERCP?
ERCP (endoscopic retrograde cholangiopancreatography) is a procedure for clearing bile duct stones using an endoscopic method. Since many patients have source gallbladder stones, the gallbladder may need to be removed surgically. In patients who prefer not to undergo surgery after ERCP, there are more problems with the gallbladder, bile duct, and pancreas. This situation is known to increase the risk of future surgery. Therefore, early gallbladder surgery is recommended after ERCP.
Conditions accompanying the patient, such as cholangitis (bile duct inflammation), cholecystitis (gallbladder inflammation), pancreatitis (pancreas inflammation), can affect the surgery process. Scientific studies show that laparoscopic cholecystectomy can be safely performed even one day after ERCP in experienced centers.
When Can a Patient with Pancreatitis Have Gallbladder Surgery?
Gallbladder stones are responsible for about 90% of pancreatic infections. A stone falling into the bile duct blocks the pancreas duct at the lower end of the bile duct, causing pancreatitis. In individuals who have experienced pancreas inflammation (biliary pancreatitis), attacks are frequent in the first 30 days, so surgery is recommended as soon as possible. Gallbladder surgery should be performed when the symptoms of pancreatitis associated with gallstones are alleviated. The surgery is recommended at the end of the period the patient has been hospitalized due to pancreas inflammation, before discharge. Gallbladder surgery performed during the same hospitalization significantly reduces problems related to stones and the risk of death.
Having experienced surgeons perform this challenging surgery will reduce the risks associated with the procedure. Gallbladder surgery can also be performed laparoscopically in individuals who have had pancreatitis. If no problems are detected after the surgery, the patient can be discharged the next day.
How is the treatment for stones that cannot be removed with ERCP?
Stones that have fallen into the bile duct may spontaneously pass into the duodenum in some patients, but in others, the clearance of the bile ducts through the ERCP (endoscopic retrograde cholangiopancreatography) method may be necessary. In the advanced endoscopic procedure of ERCP, the endoscopist reaches the ampulla of Vater (papilla) where the bile ducts open in the duodenum after which a soft wire is inserted into the bile duct. The papilla is incised and enlarged using specialized equipment. Subsequently, with equipment such as balloon or basket catheters, attempts are made to drop the stones in the bile duct into the duodenum. In some patients, it may not be possible to dislodge stones that are trapped in the bile duct into the duodenum. In such cases, the endoscopist may prefer to place stents in the bile ducts. Surgical intervention is required for stones that cannot be dislodged despite several attempts by the same or different endoscopists.
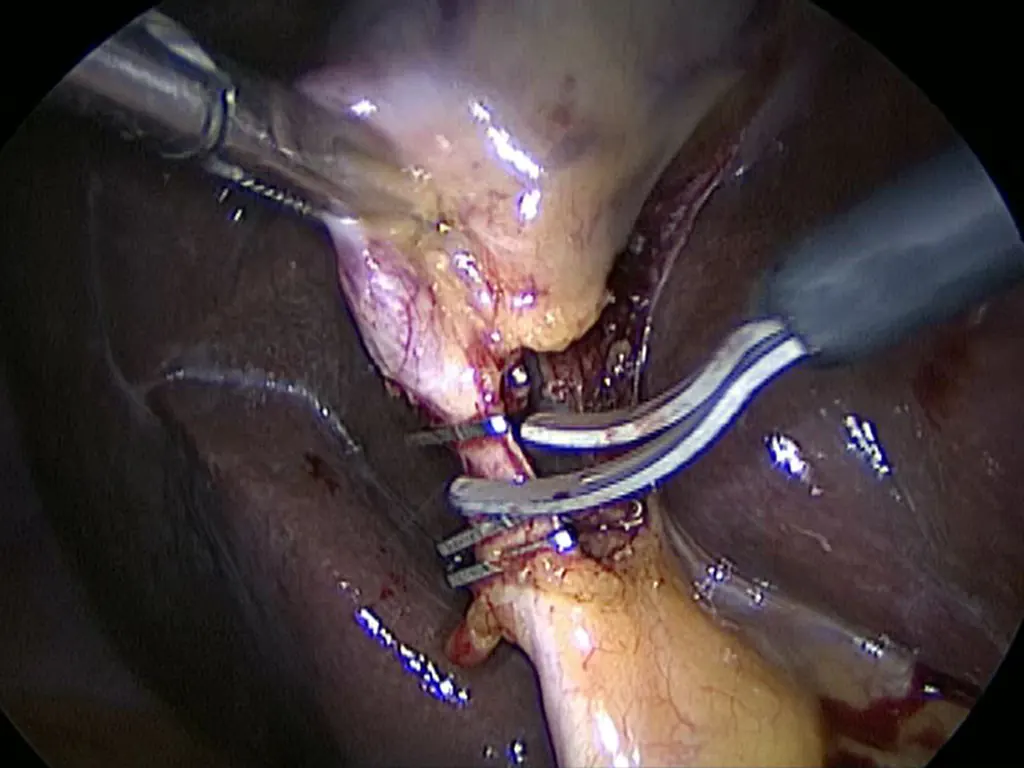
In the case of non-removable gallstones, surgical intervention can be performed using the classical open method, laparoscopic, or robotic methods. Regardless of the method used, after exposing the bile duct during surgery, an incision is made into the duct from an appropriate area to access the channel. All stones are removed through specific maneuvers, and the bile duct is cleared. After the bile duct is cleared, reconstruction of the bile duct can be performed based on the surgeon’s preference and the patient’s characteristics. This may involve direct bile duct repair, repair through T-tube, or suturing to the small intestine.
If the patient has not undergone gallbladder surgery before, gallbladder surgery can be performed in the same session to prevent future stone formation.
Various factors such as past infections, previous abdominal surgery, the location and number of stones, tissue quality, etc., can influence the duration of the surgery, which may range between 2 to 5 hours.
Patients may need to be monitored in the hospital for about 2-3 days after the bile duct stone removal surgery.
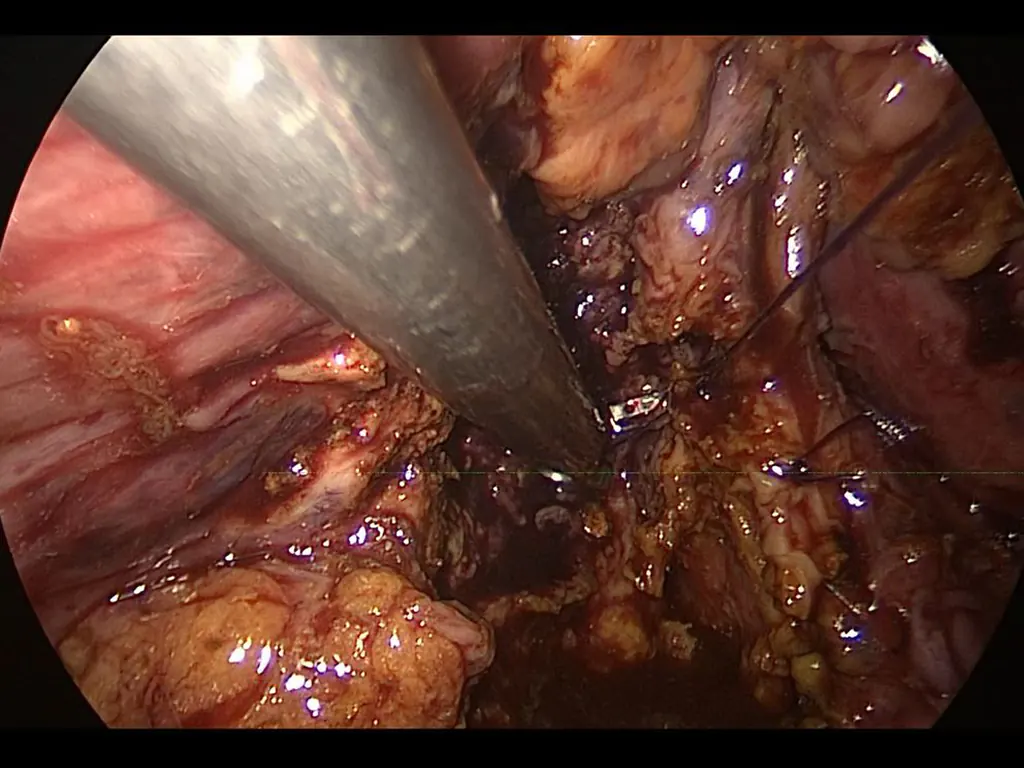
Approach to Bile Duct Injuries
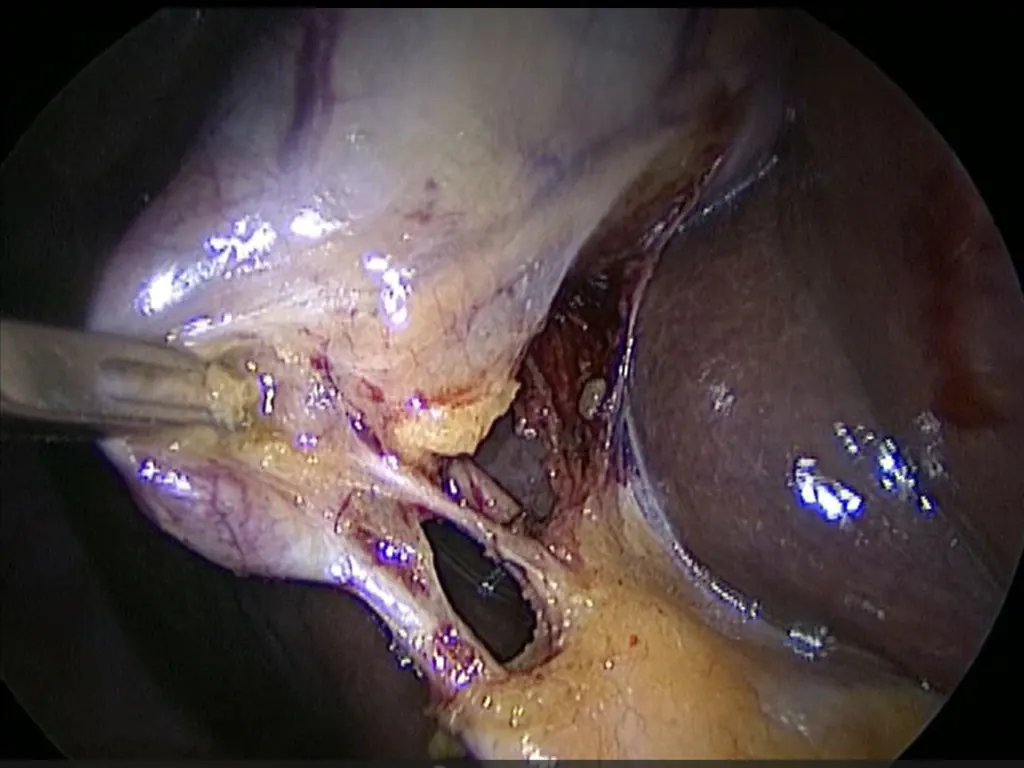
Bile duct injuries usually occur during laparoscopic gallbladder surgeries. Factors contributing to the risk of injuries during these surgeries include:
- Severe inflammation at the entrance of the gallbladder
- Very short length of the gallbladder duct
- Incorrect positioning of the gallbladder during surgery
- Anatomical abnormalities
- Inexperience of the surgeon
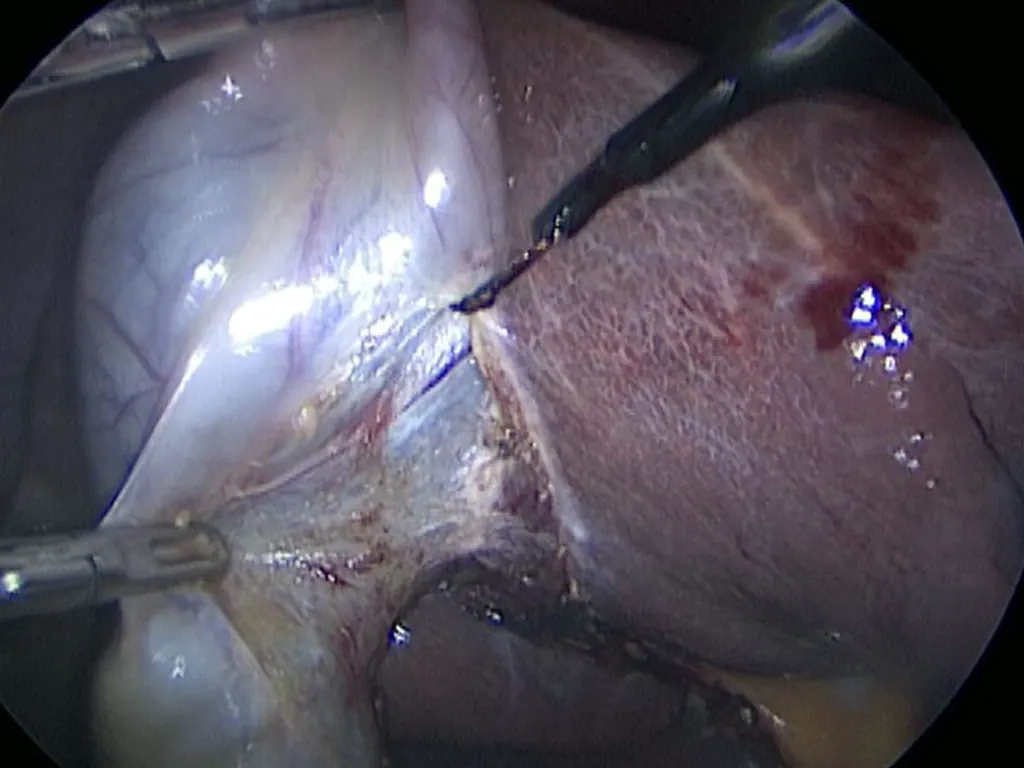
Treatment of Bile Duct Injuries
Endoscopic treatment with ERCP, repair of the bile duct, and methods such as mutual or intestinal suturing can be applied.
If the injury is identified during surgery and the surgeon is experienced, it is recommended to perform a repair intervention. In cases where the surgeon lacks experience in liver/bile duct surgery, the patient should be referred to an experienced center. Injuries are often identified after surgery, manifesting with symptoms such as bile accumulation in the abdomen or failure of bile drainage from the liver. Patients in such cases should undergo necessary examinations in experienced centers to determine the type of injury and plan appropriate interventions at the right time.
Failure to treat bile duct injuries can lead to early complications such as abscess, bile peritonitis, sepsis, and death. In the long term, it can lead to cholangitis (inflammation of the bile duct), stone or sludge formation in the bile duct, bile duct stricture, and cirrhosis.
Why do gallbladder polyps occur?
Gallbladder polyps are masses that form in the gallbladder wall due to excessive lipid and fat production. They are observed in about 5% of patients who undergo abdominal ultrasound. While most polyps are benign lesions, some carry the risk of developing into cancer. Cholesterol polyps, which are not true polyps, are the most common type and do not pose a risk of cancer. Since they cannot be distinguished from true polyps on ultrasound, they are monitored as polyps.
Adenomatous polyps are lesions that can transform into gallbladder cancer. Only 4-10% of all polyps are adenomatous. Many polyps are randomly detected on abdominal ultrasound, and some can cause abdominal pain similar to gallstones. For those with abdominal pain caused by polyps, the treatment option is gallbladder polyp surgery.
How is gallbladder polyp treatment done?
For patients without any symptoms, there is no non-surgical treatment option. The decision for follow-up or surgery is based on the risk of the polyp developing into cancer.
- Polyps larger than 10 mm carry a 43-77% risk of cancer. Therefore, gallbladder surgery is recommended for all patients with polyps larger than 10mm.
- For polyps between 6-9 mm:
- Surgery is recommended for those aged 50 and older with suspicious ultrasound findings.
- For patients under 50, biannual follow-ups are recommended for 2 years if there is no growth, followed by annual check-ups if there is no further growth.
- For polyps below 5 mm:
- For those aged 50 and older, biannual follow-ups are recommended for 2 years, followed by annual check-ups if there is no growth.
- For patients under 50, check-ups are recommended every 1-2 years.
The main problem related to gallbladder polyps is the inability to distinguish adenomatous polyps from other polyps using radiological methods. Therefore, patients with gallbladder polyps are considered in the high-risk group and are monitored. Gallbladder cancer is observed in only 1 out of every 2000 patients with gallbladder polyps.
Gallbladder polyp surgery
Surgery for polyps can be performed laparoscopically, but it has differences from a regular gallbladder surgery. In gallbladder polyp surgery:
- There should be no perforation in the gallbladder.
- Bile should not flow from the gallbladder canal to the abdominal area.
- The gallbladder should be removed outside the abdomen in a special bag.
This way, the spread of potential cancer is prevented. When the gallbladder is taken out of the abdomen, the surgeon can send it to the pathology laboratory for quick pathological examination if there are suspicions. If a pathology expert diagnoses cancer, open surgery may be required to remove a portion of the liver and lymph nodes.


